Understanding Endometriosis
This tissue reacts to hormones and can cause pain, tiredness, and other symptoms. It’s not “just bad periods” — it’s a whole-body condition.
There are three types of endometriosis, as well as adenomyosis (endometriosis within the uterus):

Endometrioma - endometriosis cyst of the ovary ('cyst' means a fluid-filled sack)

Deeply infiltrating endometriosis (DIE) - nodules at least 5mm deep

Superficial endometriosis - spots and patches that are less than 5mm deep, which can be in a single location or more widespread.

Adenomyosis - the lining of the uterus (endometrium) grows into the muscle tissue of the uterus
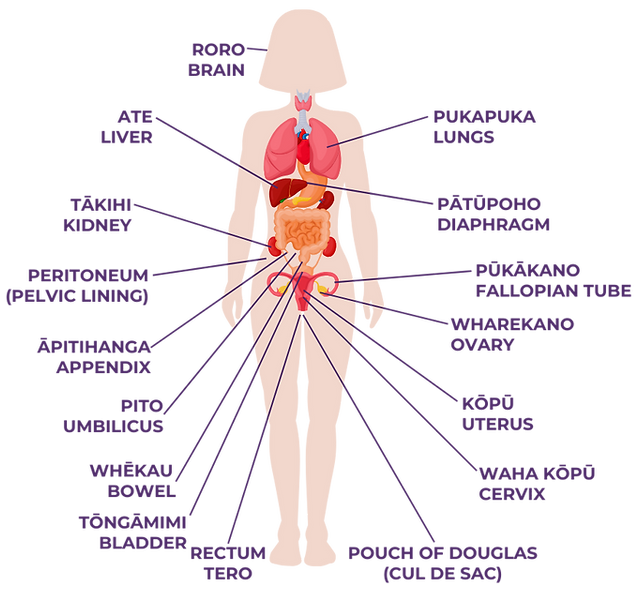
Where does endometriosis grow?
ENDOMETRIOSIS IS MORE THAN A PERIOD PROBLEM. IT'S A WHOLE-BODY CONDITION THAT CAN HAPPEN EVEN IF SOMEONE DOESN'T HAVE A UTERUS.
Endometriosis has been found in every part of the female human body and in some males. Organs that are close to the uterus are more often affected by endometriosis, such as the ovaries, fallopian tubes, pelvic lining, bowel, bladder, rectum, Pouch of Douglas and appendix.
Who can have endometriosis?
Endometriosis can affect anyone - even teens.
Endometriosis usually shows up in people of reproductive age, but it can also happen before periods start or even after menopause.
It’s not rare, and it’s not your fault. If someone in your family has endometriosis, you might be more likely to have it too.
What are the symptoms?
There are lots of symptoms of endometriosis and you do not need to have all of them to have endometriosis but the more symptoms you have, the more likely it is endometriosis causing them.
-
Pain during or around your period which affects your daily life (dysmenorrhoea)
-
Pain in your pelvic region, lower back, or legs
-
Pain during or around the time of ovulation
-
Pain going to the toilet or if your bladder is full (dysuria)
-
Bowel problems that cycle with your periods such as diarrhoea, constipation, bloating in the lower tummy or pain going to the toilet
-
Constant tiredness (fatigue)
-
Spotting before your period
-
Immune system issues - feeling run-down, getting lots of colds and taking a long time to recover
IT'S IMPORTANT TO KNOW THE SYMPTOMS OF ENDOMETRIOSIS BECAUSE EARLY DIAGNOSIS AND TREATMENT CAN HELP YOU MANAGE YOUR SYMPTOMS AND MAKE SURE THAT PAIN DOES NOT IMPACT YOUR LIFE.

How can endometriosis affect your life?
Endometriosis can affect people's lives in different ways, it isn’t just about pain.
Your symptoms might mean you need to take time off school, and they can affect how well you study or get things done.
If you have a part-time job, you might need sick days, and your work could be affected too.
Endometriosis can also impact your relationships. You might not feel like hanging out with friends, and your social life could be interrupted.
Travel or plans for moving away for study or work might be harder because of your symptoms.
All of this can affect your mental health, causing feelings of anxiety or depression.
EVERYONE EXPERIENCES SYMPTOMS OF ENDOMETRIOSIS AND PAIN DIFFERENTLY
The Pathway to Diagnosis

Identify and track your symptoms.
Book an appointment with your GP and talk to them about the symptoms you have identified and tracked. Ask your GP about an ultrasound which can help with diagnosing the cause of symptoms.
Ask your GP to refer you to a gynaecologist that specialises in endometriosis either in the public hospital or in private practice (you can also just contact one in private practice directly).
Discuss diagnosis, treatment and management options with your gynaecologist. They might suggest other tests.
Also talk with your gynaecologist about your options, including a surgery called laparoscopy where you can get a firm diagnosis as well as treatment to remove (excise) any endometriosis found.
What will happen at a GP or gynaecologist appointment?
Your GP and/or gynaecologist want to help you. Be honest about all of your symptoms and how they affect school, friends or everyday life.
Try not to be embarrassed but if you are, tell your GP/gynaecologist that you feel this way so they can help you feel at ease.
YOU MIGHT WANT TO TAKE SOMEONE WITH YOU TO YOUR APPOINTMENT. THEY CAN HELP YOU TALK TO THE DOCTOR AND ENSURE ALL OF YOUR QUESTIONS ARE ANSWERED.
TALK TO YOU SUPPORT PERSON BEFORE, SHARING WHAT QUESTIONS YOU WANT TO ASK YOUR DOCTOR AND WHAT YOU WANT AT THE END OF THE APPOINTMENT.
What questions could your GP/gynaecologist ask you?
Questions your GP/gynaecologist ask you aim to help figure out what you need, so answer honestly. Here are some questions your doctor may ask:
-
What are your symptoms?
-
When did they start?
-
Do they happen or get worse at certain times?
-
What makes them better or worse?
-
Do any of your close relatives (on either side of the family) have endometriosis or similar symptoms?
-
When did you start menstruating?
-
What is the date of your most recent period?
-
How long do your periods last and what type of flow do you experience?
-
How long is your menstrual cycle from the start of one period to the next, or is it irregular?
-
What medications, or supplements do you take on a regular basis? Have these helped with symptoms? What side effects have you experienced from these?
-
Any previous illnesses or operations?
-
Do you smoke and/or drink alcohol, and how much and how often?
REMEMBER YOUR GP WANTS TO HELP YOU SO ANSWER THEIR QUESTIONS HONESTLY. TRY NOT TO BE EMBARRASSED ABOUT YOUR SYMPTOMS AND IT'S OK IF YOU ARE. TELL YOUR DOCTOR YOU FEEL UNCOMFORTABLE TALKING AND THEY WILL HELP TO PUT YOU AT EASE
What should you ask your GP/gynaecologist?
Below are some questions you may want to ask your GP/gynaecologist:
-
What do you think is causing my symptoms?
-
What treatment options are there?
-
What do you recommend for me?
-
How will these treatments help?
-
How long do you think it will be before this treatment starts to make a difference?
-
How long do you expect me to be on this treatment plan?
-
What side effects can this treatment cause?
-
What if the treatment is unsuccessful?
-
Are there any lifestyle changes that might help?
-
What do I do if my symptoms don’t improve?
-
What will happen if I do nothing?
-
Could another condition be causing my pain and period problems?
-
What is the timeframe going forward for this treatment plan?
-
When should I have a follow-up appointment?
Are there tests to diagnose endometriosis?
There are tests your GP or gynaecologist can order to help with their diagnosis. Understanding the role of these tests may help you to advocate for yourself and keep on the right pathway for a diagnosis, treatment and management plan.
YOU CAN STILL HAVE ENDOMETRIOSIS EVEN
IF YOU HAVE A CLEAR UTLRASOUND, OR A NEGATIVE MRI
SCAN.
Treatment and Support
What treatments might my GP offer me?
To help with any pain you are experiencing, your GP
may offer you pain relief medication, suggest pain management techniques (things that you can do yourself), and/or complementary therapies as a treatment option.
Your GP can also offer hormonal treatments that may help to control symptoms and improve quality of life. The most commonly prescribed are birth control (contraceptive) pills which taken every day can help to relieve symptoms. There are many different formulations - a common one is called cerazette.
FIND OUT MORE ABOUT THE DIFFERENT TREATMENT OPTIONS BY CLICKING ON ONE OF THE BUTTONS BELOW
What pain relief medication can I take?
You can take pain relief medications, what medication you take can depend on the type of pain you are experiencing, what has caused it and where it is.
Is there anything else I can do to help with pain?
There are pain management techniques you can try to help your pain. Pain management techniques are things that you can for yourself.
What are complementary therapies and how can they help my pain?
IF YOU ARE GOING TO USE COMPLEMENTARY THERAPIES TALK TO YOUR GP FIRST TO CHECK INTERACTIONS WITH YOUR MEDICATION OR TREATMENT AND ANY SAFETY CONERNS
Complementary therapies come from lots of different types of therapists, like acupuncture, physiotherapy, osteopathy, naturopathy, massage, or Traditional Chinese Medicine.
With endometriosis, these therapies are usually used to help with specific symptoms, like period pain, or things linked to the condition, like inflammation.
If you want to try any complementary therapies, talk to your GP first to make sure they’re safe and won’t interfere with any other treatments you’re using.
While there isn’t a lot of research on complementary therapies, many people find them helpful when used along with surgery or hormonal treatments.
Can healthy movement help with my endometriosis symptoms?
Healthy movement can help with endometriosis symptoms as well as overall health and wellbeing. It's important to find what works best for you and your endometriosis, particularly if you find some types of exercise cause painful flares of symptoms.
FIND THE EXERCISES THAT YOU ENJOY AND WORK BEST FOR YOUR BODY. IT MIGHT TAKE SOME TIME AND BE A PROCESS OF TRIAL AND ERROR, BUT DON’T GIVE UP ON FINDING THE BEST PHYSICAL ACTIVITY FOR YOU!
The Ministry of Health suggests getting at least 30 minutes of exercise most days. Your activity should make you breathe a bit harder and stretch your muscles, but it shouldn’t be painful or make your symptoms worse.
Even small amounts of activity count! You can split it up into “snackercise,” like three 10-minute sessions or two 15-minute sessions. Any movement is good for you.
How do I choose a hormonal treatment?
It's important to talk with your doctor about different treatments so you can pick what works best for you and what is best for the type of endometriosis you have.
Every treatment has pros and cons, and it might take some trial and error to find what works best for you. You can combine treatments, such as Jaydess with a mini-pill to get an effective dose.
The best treatment plan can also change over time as your experience with endometriosis changes.
REMEMBER EVERYONE’S EXPERIENCE OF SIDE EFFECTS FROM HORMONAL TREATMENTS AND THE LENGTH OF TIME THESE LAST IS DIFFERENT. ALWAYS TALK TO YOUR DOCTOR OR PHARMACIST ABOUT THE PROS AND CONS OF USING MEDICATIONS AND TREATMENTS
Why is my doctor prescribing me hormonal treatments?
Hormonal treatments can help ease some symptoms. Sometimes surgery isn’t an option, the wait for surgery is long, or other health conditions make it better to manage periods with hormones. In these cases, trying hormonal treatments can be recommended.
It’s important to learn about the different options and talk to your GP about possible side effects and what taking them long-term could mean.
WHILE HORMONAL TREATMENTS ARE NOT A CURE, THEY CAN HELP WITH SYMPTOMS AND CAN BE USED SAFELY LONG-TERM. SOME TREATMENTS ARE MORE APPROPRIATE FOR SOME TYPES OF ENDOMETRIOSIS
Some studies show that using long-term hormonal treatment after surgery can lower the chance of endometriosis coming back.
Hormonal treatments can also be used with surgery, pain medication, lifestyle changes like exercise and sleep, and even complementary therapies.
The goal of hormone treatments is to:
-
Control symptoms, especially pain
-
Make day-to-day life easier
-
Reduce the risk of endometriosis coming back after surgery
Talking about Endometriosis
I'm struggling at home, school and with my friends because of my symptoms, what can I do?

It’s important to let the people in your life know about your symptoms and how they affect you. Talking to family, friends, or teachers can help them support you and offer practical help.
Sometimes it’s hardest to talk to the people closest to you, but it’s important. Pick a time and place where you can talk alone and without distractions. If you feel ready, share things like your symptoms, treatments your GP has suggested, any side effects from medication, how it’s affecting your life, and any lifestyle changes you’d like to try.
Ways your whānau and friends can support you
Here are some ideas of how people in your life can support you. You can ask them to:
Just listen to you, talking is therapeutic
Simply check-in with you about how you are doing
Brainstorm tips and tricks with you to help manage your symptoms
Understand that this is not just a 'bad period'
Acknowledge that living with these symptoms isn't easy for you
Understand sometimes plans have to be cancelled or adjusted
Help you to make lifestyle changes
Support you by coming to doctors appointments and meetings with teacher
Give you a hug
Reassure you that your relationships or friendship is unconditional
How do I talk to my teacher/s about what is happening to me?
It can be tricky to know what to tell your teachers, but to get the most out of your studies, it helps to explain how endometriosis affects you and what support you need.

Here's how you can talk to your teacher:
-
Bring a support person
Ask a parent, caregiver, or trusted adult to join you when meeting with key staff — they can help explain things and support your self-advocacy.
-
Explain what endometriosis is
Share a simple explanation of endometriosis and direct them to reliable sources like Insight Endometriosis for more information.
-
Talk about your experience
Let them know that symptoms can be different for everyone. Explain that pain and fatigue can make it hard to keep up with classwork, homework, or assignments — and that good communication is key to helping you stay on track.
-
Share what you’re comfortable with
If you feel okay doing so, talk about your specific symptoms and how often they happen. You can also share parts of your treatment or management plan if you think it will help them understand what support you might need.
-
Answer questions honestly — but on your terms
It’s okay to say “I’m not comfortable talking about
that” if a question feels too personal. Only share what feels right for you.
-
Discuss what support might look like
Talk about what might help when you’re experiencing symptoms — things like:
-
Needing toilet or rest breaks
-
Using a heat pack during class
-
Taking medication at specific times
Access to schoolwork or study-from-home options when you’re unwell
-
Make a plan together
Work with your teacher or school to create a plan for managing absences and catching up on missed work. Having a plan can help reduce stress and make things feel more manageable.
What can I do about being absent from school and missing work?

Some days, pelvic pain, fatigue, or other endometriosis symptoms might make it hard to go to school. Talk with your parent or guardian about when it’s okay to stay home and what’s manageable for you. Make sure you’re getting enough sleep, waking up early enough to get ready, having a good breakfast, and taking your medication.
Here are some ideas to address absences and missed work that you can talk about with your teacher/s:
Have a person in each class who will be responsible for contacting you with homework and assignments if you miss class.
Ask that assignments be given out in advance of any upcoming doctor appointments so that work can be completed ahead of time.
Ask your teachers to email you notes and what was done in class for the day so you don’t fall behind
Request a folder of homework and assignments to be kept in the school office so that someone can pick it up for you at the end of the day
Ask for extensions when assignments are due.
What support can I ask for when at school?
YOU DESERVE SUPPORT THAT HELPS YOU LEARN AND SUCCEED AT SCHOOL. IT'S OKAY TO ASK FOR HELP AND TO KEEP ASKING UNTIL YOU GET WHAT YOU NEED
When you talk to your teacher/s you can ask them and your school for support to help make things easier when you're experiencing symptoms. This might include changes to your timetable, help with catching up on work, or connecting with support services.
There are lots of ways your school can support you if endometriosis symptoms are making it hard to get through the day. Everyone’s needs are different, so it’s okay to ask for support that works best for you.
Here are some things you could ask for:
Ask for a toilet pass, time-out card or note so that you can leave class without needing to explain each time when you need to manage your pain, stretch or rest.
Keep your school bag light to help with your pain. Try keeping extra books at home or ask for somewhere at school to keep them.
Discuss using the sick bay or a quiet space where you can rest if your pain or fatigue gets worse.
If it's an option for your family, an out-of-school tutor can help you keep up with schoolwork so you don't feel so overwhelmed.
If the distance between classrooms is impacting, request extra time to get to classes.
Te Kura offer quality distance education through to NCEA Level 3. Find out more on their website: www.tekura.school.nz
Request flexible attendance and assignment deadlines so you can keep up with work or catch up on anything you have missed.
Connect with Disability Support, Stress Counselling or other services at your school, they can work with you and your whānau to make a plan.
Find out where you can fill a hot water bottle or get a heat pack ready that you can then use through the day to help with your pain.
Seek support from the school counsellor to talk things through and find strategies to cope.
Plan with your physical education teacher modified activities that won't make your pain worse. Exercise can help but it's important it's the right movement for your body.
Find a trusted teacher that you can check in with on a regular basis and discuss what support you need.
The school can also apply to the Ministry of Education for you to sit your external exams separately to others so that you can get up and walk around.
You don’t need to ask for everything at once. A good first step is talking to a teacher or school staff member you trust. You deserve to feel supported at school — and you’re not alone.
Your Mental Wellbeing
How do I look after my mental well-being when I'm in pain?
FOR MANY OF US, WHEN WE TALK ABOUT MENTAL HEALTH WE'RE THINKING ABOUT MENTAL ILLNESS OR MENTAL DISTRESS. BUT LIKE PHYSICAL HEALTH, MENTAL HEALTH IS SOMETHING WE ALL HAVE, AND WE NEED TO LOOK AFTER IT. MENTAL WELL-BEING IS ABOUT FEELING GOOD, FUNCTIONING WELL, AND FEELING CONNECTED.
Living with pain can affect your mood and in turn affect your perception of pain. It's often described as a cycle where your pain causes feelings of anxiety, low mood, fatigue, and sleeplessness, which can result in increased pain.
The increased pain can then cause a low mood, tiredness, and stress, so you can get caught in an endless cycle. But there are ways to break the cycle and reclaim your sense of well-being.
Here are some things you could try to look after your mental well-being and be helpful in managing your pain:
What else can I do to look after my mental well-being?

Looking after your mental well-being is just as important as caring for your physical health. Self-care is one way to do that — it’s about doing small, intentional things that help you feel more like yourself. And self-care doesn’t look the same for everyone!
Self-care is more than bubble baths or taking a break (though those things are great too!). It’s about paying attention to what helps you feel balanced, calm, and cared for — especially when life gets tough. Self-care can look different for everyone, and there’s no “right” way to do it. The important part is choosing things that help you feel supported.
There are six types of self-care — try different ideas and see what feels good for you:
Physical self-care
-
Getting enough sleep
-
Stretching
-
Gentle movement
-
Drinking water
-
Using a heat pack
-
Resting when you’re in pain.
Emotional self-care
-
Writing in a journal
-
Talking to someone you trust
-
Naming your feelings
-
Listening to music that matches your mood
-
Creating art to express your feelings
-
Practicing self-kindness
Spiritual self-care
-
Spending time in nature
-
Exploring your values or beliefs
-
Meditating
-
Doing something that helps you feel connected and grounded
Social self-care
-
Spending time with friends or whānau who make you feel safe and supported
-
Joining a club, group, or online community
-
Spending time with someone who 'gets it'
-
Reaching out, even when it's hard
Intellectual self-care
Do something that make you curious or focused:
-
Reading
-
Drawing
-
Doing a puzzle
-
Learning something new
Sensory self-care
Calm your senses with:
-
Soft textures
-
A warm shower
-
Gentle music
-
Something that smells nice — like lavender or your favourite food
If you are worried about how often you are getting your period, any pain you are having, or other symptoms before, during or after your period you can talk to your school nurse, GP or another healthcare prover.
Here is what to do next if your period pain is really bad, doesn't get better with pain medicine, lasts more than the first few days of your period or is affecting your daily life:
Visit our Info Hub
On our Info Hub you’ll find more information guides that explore endometriosis and related topics in greater depth. These can be especially useful if you’d like a deeper understanding or if you’re looking for resources to share with whānau, teachers, or health professionals.
This webpage is also available as a free downloadable guide: Endometriosis: A Guide for Teens. You may also find Understanding Periods: A Guide for Teens helpful.

Join us in our mission to empower people with endometriosis and improve the lives of thousands in Aotearoa New Zealand
We rely on the support of our community to provide the resources and support that people with endometriosis need. There are many ways to get involved and make a difference, from making a donation to volunteering your time.










